
For people with Attention Deficit Hyperactivity Disorder (ADHD), autism, or other forms of chronic cognitive impairment, the built environments they occupy often compound the everyday challenges their conditions present. This environmental inequity impacts a staggering number of Americans, and it is an issue that Stuart Shell, architect and building scientist at BranchPattern, believes architects and planners should work hard to address. In this piece, Stuart suggests ways designers can make themselves better advocates for the cognitively-impaired, while advancing a notion central to building a more equitable world: design that works for the most vulnerable among us is design that works well for all of us.
Too often our cultures, along with the cities we build, assume we all have the same backgrounds and abilities. Today our buildings are overwhelmingly built on a foundation of ableism, with urban form deferring primarily to able-bodied persons. This ideology is so widespread as to make invisible the barriers in the built environment experienced by the one in five individuals living with cognitive impairments.
The most common reason for cognitive impairments is a mental disorder: Alarmingly, over 20% of Americans have one. And outside of a psychological diagnosis, there are many reasons why people might suffer from persistent cognitive impairments—neurological disorders such as Alzheimer’s or dementia affect one in five people over 71 years old, or 1.3% of all Americans.1 Diseases such as rheumatoid arthritis, Down syndrome, cerebral palsy, and conditions like migraines can also diminish cognitive abilities.
Cognitive impairment often involves deficits in executive function: the skill required to control and coordinate all of the brain’s cognitive abilities and behaviors, like a CEO overseeing all departments in a business to make sure they progress efficiently and effectively.2 There are many theories about the nature and operation of executive functioning,3 but what might be the implications for design and planning? Take the example of ADHD. Decreased activity in the hippocampus—specifically, low dopamine levels—appears to be why individuals with ADHD exhibit impulsive behavior. Providing engaging sensory environments that promote dopamine production in the brain may be a helpful support in stimulating prefrontal brain activity.
It’s imperative for architects to make streets and buildings more adaptable to everyone’s use. When our designs fall short of these standards, we risk making arbitrary barriers for individuals with cognitive impairments. But despite the physical environment having direct and indirect impacts on cognition,4 cognitive impairment is rarely considered as a design criterion, and practitioners in planning and design typically lack the lexicon to discuss inclusive design. (See the glossary below for a crash course.) From my perspective as an architect, questions about access for individuals with impairments typically go unasked, short-circuiting a design process that could remove barriers. Instead of lumping together “accommodations” for the “disabled,” we should ask which type of impairments people will bring with them to our buildings, streets, and parks. We have a mandate to expose and reduce these barriers so that the environment can help fulfill rather than hinder our potential. This means not only making the built environment more accessible but also increasing access to nature, providing the diversity of surroundings that humans need to thrive physically and mentally. Re-imagining our built environment in collaboration with individuals with cognitive impairments will be a step toward a more inclusive society, resulting in cities that improve the mental well-being of the entire population.
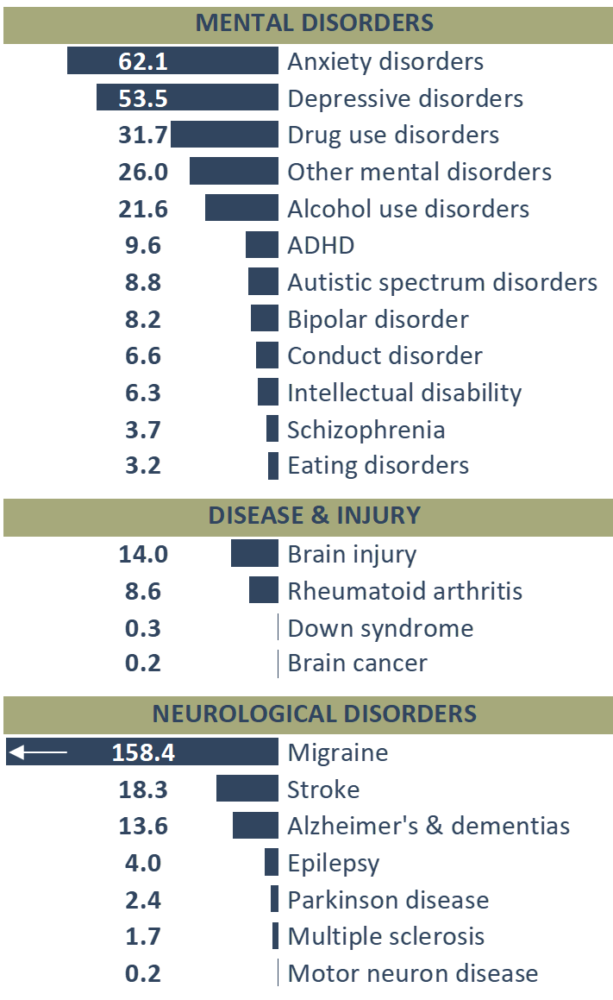
Table 1:
Prevalence per 1000 (2016, United States)
Data source: Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2017. http://ghdx.healthdata.org/gbd-results-tool.
Design for cognitive impairments is also a matter of equity. The legislative wins of the civil rights movement in the 1960s helped set the stage for those with physical impairments to advocate for their rights to access the built environment. Design improvements that address these impairments can now be thought of as universal design. Popularized in the 1980s, universal design posits that buildings, products, and processes work better the more people can use them. Undergirding universal design is an agenda that seeks to restore agency to excluded groups and to confront the ableist bias in society. This makes proponents of universal design also activists for social change.
The Americans with Disabilities Act (ADA) legislation of 1990 is a great starting point, but despite increased awareness of cognitive impairments, designers still lack a framework for creating solutions and incorporating the tenets of universal design into practice. Removing obstacles in the built environment, for instance, such as those prescribed by the ADA, is not sufficient for creating designs that address cognitive impairments. A more salutogenic approach to mental health in the built environments—focused on promoting health and well-being rather than preventing disease or harm—provides opportunities for rich, physiological interactions, like chances to modify our surroundings to suit our mental and physical needs. Enabling people to access the built environment in this way helps exercise executive functioning skills: The choice of which path to take or which room to use provides a sense of control. This concept of manageability gives people the opportunity to create healthy outcomes while maintaining a strong sense of self.5 Adaptability is a hallmark of good design because it helps people accomplish their goals in a way that works for them.
Providing all persons with options and the freedom to choose among them isn’t just a good idea—it’s also inherently pleasurable. Alliesthesia, the desire to achieve a neutral internal state, explains why water tastes better when we’re thirsty, and quiet is more desirable when we’re stressed.6 Providing arenas for people to exercise their executive functioning skills can create more opportunities for pleasure in the built environment.
Encouraging agency and mental exercise within our surroundings is one way the built environment can support mental health. Attending to the ways a given suite of cognitive impairments compromise agency can help designers identify avenues for intervention. For instance, individuals with autism spectrum disorder (ASD) have symptoms that vary widely, although problems with social interactions are typical. Many individuals with ASD also have trouble with sensory integration—meaning they may be overwhelmed by lights, noise, and touch. Deficits in executive function are common. Given these characteristics, some simple accommodations could improve the learning experience for a student with ASD in a mainstream classroom, for example. Having an alcove in the room available for sensory escape would help ease overstimulation. Allowing options for self-regulation can help individuals with ASD practice executive functioning skills.7 Increased ventilation, insulation from outdoor noises, and controllable lighting are also particularly beneficial. The resulting classroom, tailored for those with ASD, also clearly stands to help everyone focus.
Down syndrome is the most common form of genetic cognitive disability. It is characterized in part by atypical development of the prefrontal cortex, often producing deficits in executive function. While driving a car is out of reach for many individuals with Down syndrome, taking the bus is often a viable option. Navigating a transit system, however, can be a multi-step process that taxes our executive functioning, attention, and memory skills. Viewing this as an accessibility problem, there are several ways that attending to the nuances of this population could translate into better transit design. Bus stops with clear signage, a place to sit, and dynamic arrival times would reassure riders that they are at the right place while reducing attention demands. A digital interface at the bus stop where riders can enter their destination would confirm their travel plans and arrival time. The same interface could accept payment for the trip, easing a barrier to boarding the bus and finding a seat. A transit system designed in consideration of riders with cognitive impairment has features that all users would enjoy, allowing them to focus on alternate tasks and enjoy the ride.
Urban design is a powerful avenue for mental health interventions, but being able to escape the city is equally important. The complexity of our brains can lead to an array of sensitivities when it comes to pollution in the air and water. Exposure to higher concentrations of dust, endocrine disruptors, and carcinogens may explain some differences in mental health for city-dwellers.8 Some research has shown that the incidence of autism spectrum disorder appears to be higher in cities.9 Anthropogenic soundscapes and lighting also disrupt sleep, increasing the risk of depression and other mood disorders.10 Just the stress from the pace of life in developed areas is associated with more pronounced symptoms for some individuals with cognitive impairment.11 This evidence supports the hypothesis that ecology is linked with mental health.
Spending time in nature positively affects everyone’s mood, and is particularly impactful for those with mental disorders.12 Children who live nearby nature are also more psychologically resilient to stressors in life.13 A patch of wilderness can provide seminal developmental experiences for children, while also giving everyone room to breathe—literally and figuratively. Adding green space to our cities is a common-sense strategy for combating light and noise pollution, helping us entrain healthy sleep cycles. The evidence is telling us that better design for cognitive impairment means engineering with ecological principles that reduce pollution and increase our exposure to living things.14
For those with cognitive impairments, design for brain health is a civil rights issue. Neurotypical designers—those without neurologically atypically patterns of thought and behavior—have a mandate to combat the ideology of ableism and take part in the lived experience of their neighbors with cognitive impairments. This in part requires an earnest effort to include individuals with impairments—by including disability advocates as stakeholders in urban development. Recognizing exceptional projects that also meet the needs of those with disabilities will raise awareness of the damage caused by ableist development. Ultimately we could see rating systems such as Leadership in Energy and Environmental Design (LEED) incorporate metrics for inclusive design, improving the standards of design in our communities overall.
The brain activities that underpin success—executive function, memory, and attention—reside within all of us. Designing for these activities from multiple perspectives expands our knowledge of how our brains work, helping build empathy and, hopefully, a more cohesive community. Designing spaces for those with cognitive impairments supports neurotypicals too, building a future city that’s designed with all of us in mind.
Ableism
A common belief that individuals with impairments are abnormal and inferior to “able-bodied” people. Common ideas associated with this ideology are that individuals with impairments have less opportunity in life and suffer from limitations on their development as a whole person. Our buildings and streets bear testament to the hegemony of this ideology.
Cognitive Impairment
This umbrella term indicates deficit in brain function observed through behavior. This article focuses on problem-solving skills (executive functioning), attention, and working memory. Intellectual disability and learning disability are common types of cognitive impairment.
Disability
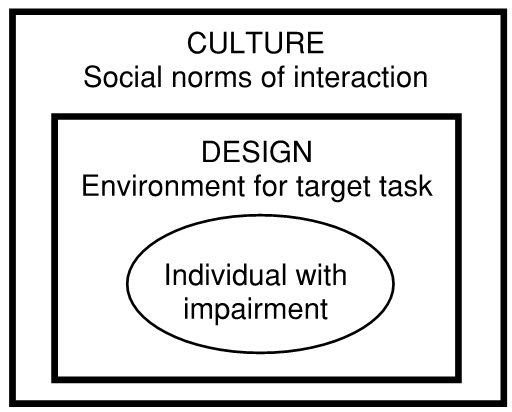
Individuals experience a disability when they are unable to perform their intended task. Tasks with social significance such as going to work and self-care add definition to the disability a person experiences. Sometimes tasks with little relevance to everyday life such as standardized tests are used to label a person with a disability. Having an impairment does not mean a person has a disability. Accommodations can eliminate barriers to participation. Eyeglasses can give an individual with poor vision the ability to drive, just as a wheelchair can enable someone with cerebral palsy to go shopping. Social norms and the design of the environment create barriers that act on a person’s impairment, thereby creating the disability.
DSM 5
Diagnostic and Statistical Manual of Mental Disorders (DSM), published by the American Psychiatric Association. This book is the basis for classifying mental disorders. It describes differences (and similarities) in cognitive functioning for disorders.
Impairment
Difficulty hearing, a migraine, and a broken arm are examples of impairments. They may be temporary, situational, or persistent. All of us will experience impairment at some time—for example, having our eyes dilated for a new pair of eyeglasses or having vision that needs correction in the first place.
Neurodiversity
The concept that many “disorders” such as autism, attention deficit and hyperactivity disorder (ADHD), post-traumatic stress disorder (PTSD), and schizophrenia are best explained as natural variation in neurology. This is supported by the evidence that individuals on the autism spectrum may be high-functioning, such as Temple Grandin and Albert Einstein. Neurodiversity is also a social movement.
Person with Disability
Disability is a social phenomenon and is not inherent in the individual. That is why we refer to someone “with a disability” and not a “disabled” person. A person is determined to have a disability by culture, not by their impairment. While “people first” language is accepted in the United States, many activists do refer to the “Disabled” to emphasize group identity and a shared experience of ostracism and discrimination.
Salutogenic
This term was introduced by Aaron Antonovsky in 1979 to describe how health is created through interactions with the social and physical environment. It is distinct from the dominant model in medicine, which presumes that health is the absence of pathogens. Comprehensibility, manageability, and meaningfulness are the key components of a sense of coherence that ultimately determines health.
Social Security Disability Insurance (SSDI)
In the United States, many of us think of disability in the context of federal assistance. In fact, only one in five individuals with a disability receive SSDI. Of those who do, psychiatric disability is the largest group receiving benefits.
1. B. L. Plassman, K. M. Langa, G. G. Fisher, S. G. Heeringa, D. R. Weir, M. B. Ofstedal & R. B. Wallace, “Prevalence of cognitive impairment without dementia in the United States,” Annals of Internal Medicine 148, no. 6 (Mar. 18, 2008): 427-434.
2. “Executive Functions,” UCSF Aging and Memory Center, accessed April 18, 2019, https://memory.ucsf.edu/executive-functions.
3. For a detailed review, see S. Goldstein, J. A. Naglieri, D. Princiotta & T. M. Otero, “Introduction: A History of Executive Functioning as a Theoretical and Clinical Construct,” in The Handbook of Executive Functioning (Springer, New York, 2014), 3-12.
4. For an overview of mental health and design, see G. W Evans. “The Built Environment and Mental Health,” Journal of Urban Health 80, no. 4, (2003): 536-555.
5. J. A. Golembiewski, “Start Making Sense: Applying a Salutogenic Model to Architectural Design for Psychiatric Care,” Facilities 28, no. 3/4 (2010): 100-117.
6. For a detailed discussion of alliesthesia, see M. Cabanac, “Physiological Role of Pleasure,” Science 173, no. 4002 (1971): 1103-1107.
7. For a detailed discussion of classroom design for ASD, see M. Mostafa, “An Architecture for Autism: Concepts of Design Intervention for the Autistic User,” International Journal of Architectural Research: ArchNet-IJAR 2, no. 1 (2008): 189-211.
8. For example, see J. A. Ailshire & E. M. Crimmins, “Fine Particulate Matter Air Pollution and Cognitive Function Among Older U.S. Adults,” American Journal of Epidemiology 180, no. 4 (2014): 359-366 and L. G. Costa, T. B. Cole, J. Coburn, Y. C. Chang, K. Dao & P. J. Roqué, “Neurotoxicity of Traffic-Related Air Pollution,” Neurotoxicology 59 (2017): 133-139.
9. A correlation between ASD and degree of urbanicity is shown in M. B. Lauritsen, A. Astrup, C. B. Pedersen, C. Obel, D. E. Schendel, L. Schieve & E. T. Parner, “Urbanicity and Autism Spectrum Disorders,” Journal of Autism and Developmental Disorders 44, No. 2 (2014): 394-404. A correlation to air pollution is shown in T. A. Becerra, M. Wilhelm, J. Olsen, M. Cockburn & B. Ritz, “Ambient Air Pollution and Autism in Los Angeles County, California, Environmental Health Perspectives 121, No. 3 (2012): 380-386.
10. For a discussion of urban lighting and mental health, see R. Chepesiuk, “Missing the Dark: Health Effects of Light Pollution,” Environmental Health Perspectives 117, No. 1 (2009): A20.
11. E. Gullone, “The Biophilia Hypothesis and Life in the 21st Century: Increasing Mental Health or Increasing Pathology?” Journal of Happiness Studies 1, No. 3 (2000): 293-322.
12. For example, see J. Barton & J. Pretty, “What is the Best Dose of Nature and Green Exercise for Improving Mental Health? A Multi-Study Analysis,” Environmental Science & Technology 44, No. 10 (2010): 3947-3955 and P. Grahn, A. M. Pálsdóttir, J. Ottosson & I. H. Jonsdottir, “Longer Nature-Based Rehabilitation May Contribute to a Faster Return to Work in Patients with Reactions to Severe Stress and/ or Depression,” International Journal of Environmental Research and Public Health 14, No. 11 (2017): 1310.
13. See N. M. Wells & G. W. Evans, “Nearby Nature: A Buffer of Life Stress Among Rural Children,” Environment and Behavior 35, No. 3 (2003): 311-330.
14. See G. N. Bratman, J. P. Hamilton & G. C. Daily, “The Impacts of Nature Experience on Human Cognitive Function and Mental Health,” Annals of the New York Academy of Sciences 1249, No. 1 (2012): 118-136.
15. For a foundational article on the role of culture in creating disability, see R. McDermott & H. Varenne, “Culture as Disability.” Anthropology & Education Quarterly 26, No. 3, (1995): 324-348.
16. M. B. Mittelmark, “Introduction to the Handbook of Salutogenesis,” in The Handbook of Salutogenesis (Springer, Cham, 2017), 3-5.
With VAR 20, we explore the often hidden connection between mental health and urban environments. We hope this issue makes people more aware of the many ways our cities impact our health, our brains, and our lives. This article is the third piece featured in VAR 20. To receive future articles and interviews from Van Alen Report, please subscribe below.
SUBSCRIBE